Respiratory System
Introduction
Even at rest, the human body requires a large amount of oxygen to fuel the metabolic pathways that generate ATP. The respiratory system facilitates the exchange of gases between the atmosphere and blood to deliver oxygen to tissues while removing one of the end products of metabolism, carbon dioxide. The interface between air and blood in the respiratory system is composed of fluid and tissue (cells and extracellular matrix). Gases must dissolve in this fluid and the pass through the tissue barrier to move between air and blood.
Gases diffuse passively between air and blood, and knowing some of the parameters that determine the rate of diffusion between air and blood help to understand the structure of the respiratory system. Fortunately for us, a formula, shown below, describes the rate of diffusion of gases between air and blood.

Though it has several terms, the formula is quite simple and contains two terms that relate to the structure of the respiratory system. The formula states that the rate of diffusion between air and blood across a tissue barrier depends upon the surface area of the barrier (A) and the thickness of the barrier (a). Based on the formula, the respiratory system facilitates gas exchange by creating a tissue barrier that has a large surface but is very thin.
To generate a large surface area, the respiratory system consists of a highly branched network of tubes that end in thin sacs that separate air from blood. The respiratory system starts with a single tube, called the trachea, that is approximately 2 cm in diameter and through 23 generations of branching produces millions of small sacs called alveoli that create an internal surface area of approximately 50 to 75 m2 (roughly the size of tennis court). In addition, the rate of diffusion is inversely related to distance. To facilitate gas exchange, the walls of alveoli have a very thin layer of tissue that separates air and blood.
The network of tubes in the respiratory system is divided structurally and functionally into conducting airways and respiratory airways.
- Conducting airways comprise nose, pharynx, larynx, trachea, bronchi, and bronchioles. These segments serve to conduct, clean, warm, and moisten the air. This lab will discuss conducting airways starting from the trachea.
- The respiratory (exchange) airways comprise respiratory bronchioles, alveolar ducts, alveolar sacs, and alveoli. These segments facilitate gas exchange and are located entirely within the lung.

As we describe the structure of the segments of conducting and respiratory airways, keep in mind these questions. How does the epithelium of the segment serve the function of the segment? What structures keep the airways open or regulate their diameter? How does the respiratory system handle the large number of foreign particles that we inhale?
Conducting Airways - Sections
The structure of the conducting airways serves its primary functions of facilitating flow into and out of the respiratory portion of the airway and conditioning and cleaning the air that enters the lung. Conditioning mostly involves moistening the air by creating a fluid layer on the surface of the conducting airways. Cleaning the air is achieved mostly through a layer of mucus on the surface of the conducting airway that traps inhaled particles. Cilia on the apical surface of some of the epithelial cells in the conducting airway move the mucous upward through the respiratory tract.
The conducting airways start with the nose, pharynx and larynx. We start our discussion with the trachea.
Trachea
The trachea connects the larynx above and the two primary bronchi below. The trachea is easily identified by its large C-shaped hyaline cartilage rings. These rings prevent the collapse of the tracheal mucosa during inspiration and reside on the anterior side of the trachea. The ends of the rings are bridged by the trachealis muscle, which is composed of smooth muscle fibers, on the posterior side of the trachea. Note the presence of glands in the submucosal layer of the trachea. These glands contain cells that secrete mucous and others that secrete fluid that is roughly isotonic with plasma. The fluid is released onto the surface of the epithelium. The epithelium in the trachea is pseudostratified.

The image below shows in higher magnification the components found in the wall of the trachea and large bronchi . The epithelium facing the lumen of the trachea is clearly pseudostratified with cilia and is discussed in more detail below. The epithelium rests atop a thick basement membrane. Beneath the basement membrane is the lamina propria that contains connective tissue and blood vessels. The epithelium, basement membrane and lamina propria compose the mucosal layer.

The submucosa resides below the mucosa and contains a large number of seromucinous glands. The glands secrete fluid and mucus onto the surface of the epithelium. The vapor from the fluid on the epithelium moistens the air which will help prevent desiccation in the alveoli when the air reaches that point. Note also the hyaline cartilage in the submucosa. In the trachea, the cartilage forms a C-shaped ring on the anterior side of the trachea. In bronchi, the cartilage forms plates.
Pseudostratified Epithelium of Trachea and Bronchi
The trachea and bronchi are lined by pseudostratified epithelium. The main function of the pseudostratified epithelium is to trap and remove airborne foreign particles and pathogens that enter the lung during inhalation. The image below shows a section of the wall of a bronchus at higher magnification. Note the characteristic pseudostratified epithelium that contains ciliated cells and mucus-secreting cells. Mucus is a mix of water, ions a variety of glycoproteins called mucins and several other proteins. Mucins form a gel-like structure on the surface of the epithelium that traps foreign particles and pathogens. In addition, the components of mucus contain anti-oxidant, anti-microbial and anti-protease activities. The cilia on the apical surface of the pseudostratified epithelium beat in a wave-like fashion to move mucus upward through the respiratory tract. Cilia are filled with microtubules. The motor protein dynein resides at the base of cilia and slides the ciliary microtubules against each other to generate cilia motility.

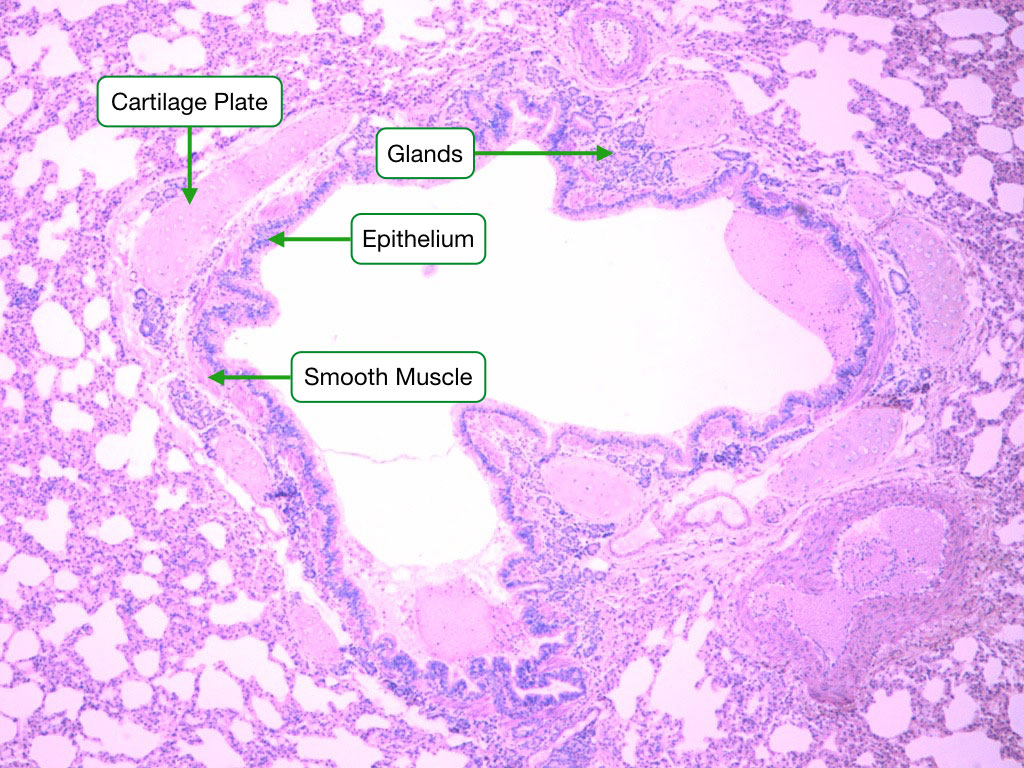
Bronchi
Two main bronchi branch from the trachea to supply the left and right lung. Main bronchi branch again to form secondary bronchi, and the branching process continues for 9 more generations to form smaller and more numerous bronchi. Larger bronchi contain a pseudostratified epitheium with similar cellular composition as the trachea, but as bronchi decrease in size, the epithelium becomes ciliated columnar and the number of goblet cells decreases. The basement membrane in bronchi is much thinner than in the trachea. Glands, similar to those in the trachea, are still found in the submucosa.
Bronchi are distinguishable in sections of lung tissue by the cartilage plates in their walls. When the bronchi enter the lung, the C-shaped cartilages that characterize the trachea and primary bronchi are replaced by irregular plates of cartilage that surround the cylindrical muscular airway tube. As in the trachea, the cartilage prevent collapse of bronchi. Bronchi also contain a layer of smooth muscle that is arranged spirally. The significance of the spiral arrangement is unclear but contraction of the muscle reduces the diameter of bronchi.
Conducting Bronchioles
Conducting bronchioles are the final segment of conducting airways, composing the 11th to 16th generations of the respiratory system. The diameter of conducting bronchioles is usually 1 millimeter or smaller. The epithelium of conducting bronchioles is ciliated columnar with very few goblet cells. Bronchioles lack cartilage plates and glands, distinguishing them from bronchi.
The lack of cartilage would make bronchioles susceptible to collapse during expiration and subsequently difficult to open during inspiration. To keep bronchioles open during the respiratory cycle, the tissue surrounding and attached to the walls of bronchioles generates tension mostly from the components in its extracellular matrix. Note that most of the tissue surrounding bronchioles is alveolar. As alveoli expand during inspiration, the tension in the walls of the alveoli is transmitted to the walls of bronchioles to expand them. During expiration when transmural pressure falls, the stiffness of alveolar walls prevents bronchioles from collapsing. Diseases that damage the walls of alveoli reduce the tension on bronchioles, making them more difficult to open and increasing the resistance to airflow through bronchioles.

Bronchioles also display a layer of smooth muscle that can change the diameter of bronchioles under certain conditions to decrease or increase airflow resistance. Parasympathetic nerves release acetylcholine onto bronchiole smooth muscle cells to stimulate contraction and decrease the diameter of bronchioles. In contrast, sympathetic nerves release norepinephrine which relaxes bronchiole smooth muscles and widens the diameter of bronchioles. Epinephrine, produced in the adrenal gland, has a similar but more powerful effect as norepinephrine.
The size of the smooth muscle layer can also change under certain disease processes. Both asthma and other inflammatory responses have been shown to increase the thickness of smooth muscle layer in bronchi and conducting bronchioles through both hypertrophy and hyperplasia. The thicker muscular layer increases airway resistance, reducing air flow into the respiratory airways.
The smallest conducting bronchioles are called terminal bronchioles which transition into the respiratory airways.
Respiratory Airways
The respiratory airways extend from the respiratory bronchioles to the alveoli. The primary function of this section of the respiratory tract is to facilitate gas exchange.
The respiratory bronchioles branch from terminal bronchioles and compose the 17th to 19th generations of branching. Respiratory bronchioles have a diameter of about 0.5 mm and contain a few alveoli scattered along their walls. Each respiratory bronchiole branches into 2 to 11 alveolar ducts that retain a cuboidal epithelium and still contain smooth muscle fibers in their walls. Along the walls of alveolar ducts are single alveoli and numerous alveolar sacs that comprise 2 to 4 alveoli. The space at the entrance from the alveolar duct to an alveolar sac is referred to as the atrium.

The epithelium of respiratory bronchioles is cuboidal with a mix of ciliated cells and club cells. Club cells perform several important functions, including production of material similar to surfactant, detoxification of inhaled chemicals, and absorption of ions and water from the airway lumen to control the amount of fluid in the airway. Club cells also serve as stem cells that are capable of replacing the other epithelial cells in respiratory bronchioles.
Alveoli
Alveoli facilitate the exchange of gases between inhaled air and blood by creating a thin tissue layer between air and blood. The tissue layer consists of the airway epithelium, basement membrane and endothelium of the capillary. The combination of thin barrier between air and blood and large alveolar surface area allow for rapid diffusion of gases between air and blood.
When viewing histological images of alveoli and thinking about the process of gas exchange, it’s important to keep in mind that the surface of alveoli that faces the air space is covered by fluid. This fluid is usually not evident in histological images but its presence has important consequences for gas exchange and the structure of alveoli. First, oxygen in the air must dissolve in the fluid before diffusing across the walls of alveoli. At 37˚ C, the solubility of oxygen in water is about 0.0013 mM/mm Hg. Second, the amount of fluid in the alveoli will also affect the rate of diffusion of gases between the airway and blood. The more fluid present, the greater the distance that gases must travel between air and blood. The epithelial cells of alveoli reduce the amount of fluid in the lungs through active reabsorption of sodium and chloride from fluid in the lumen. The osmotic gradient created through reabsorption of sodium and chloride draws water from the airway of the alveoli into the interstitium. Lastly, fluid affects the architecture of alveoli. The interface between fluid and air generates surface tension that is sufficiently strong to collapse alveoli. Surfactant, described below, reduces surface tension to prevent collapse of alveoli.
Cells of Alveoli
Alveoli contain several different cell types which can be divided into resident cells and transient cells. Resident cells are those that create the structure of alveoli and participate in gas exchange. Resident cells include pneumocytes, endothelial cells and the occasional fibroblast. Transient cells include dust cells (macrophages) and other immune cells that vary in number depending on the presence of infectious agents and foreign particles.
Pneumocytes
The surface (air-facing) epithelium of the alveoli contains two developmentally related but functionally distinct cells, known as pneumocytes. Type I pneumocytes form a simple, squamous epithelium that cover the vast majority of the surface area of alveoli. Type I pneumocytes surround a basement membrane and endothelial cells of capillaries to form the air-blood barrier, across which gases diffuse between air and blood.

Type II pneumocytes are larger, cuboidal cells. They produce and secrete surfactant into the fluid that faces the air space. Surfactant reduces the surface tension along the fluid-air boundary, preventing alveoli from collapsing. Surfactant contains molecules similar to lipids in that they contain hydrophilic and hydrophobic domains (amphiphilic). The hydrophobic domains interact with air while the hydrophilic domains associate with the fluid. Surfactant also contains protein components that function in innate immunity in addition to playing structural roles in the formation of surfactant.
Type II pneumocytes are often found in the junctions between to alveolar walls. After damage to alveoli, type II pneumocytes are capable of proliferating and differentiating into type I pneumocytes during the repair process.
Although type II pneumocytes are more numerous than type I pneumocytes, type I pneumocytes occupy about 95% of the surface area of alveoli because of their squamous shape.
Pneumocytes EM
Electron micrographs reveal the structural differences between type I and type II pneumocytes and the thinness of the barrier that separates the airway from the circulatory system. Note the thin cytoplasm of the type I pneumocyte that surrounds a capillary. The capillary is defined by a continuous endothelium. Between the endothelial cell and type I pneumocyte is a thin basement membrane that is shared by both cells. The size of the red blood cells in the capillary allows you to estimate the distance across which gases diffuse between the airway and blood.

Type II pneumocytes are considerably larger and more cuboidal than its type I counterparts. The lamellar bodies are distinct features of type II pneumocytes and contain the phospholipid precursors to pulmonary surfactant, which will be released into the fluid in the airway to reduce the surface tension between the fluid and air.
Air-Blood Barrier
This electron micrograph shows the three lays of the air-blood barrier across which gas exchange occurs. The type I pneumocyte is part of the simple squamous epithelium of the alveolus and the endothelial cell represents the capillary epithelium. The two cells share a fused basement membrane, which allows for the minimization of the barrier across which exchange of gases occur. Oxygen in the air dissolves into the fluid on the surface of alveoli and then diffuses through the cytoplasm of type I pneumocytes, across the basement membrane and then through the cytoplasm of the endothelial cell to reach the blood. Carbon dioxide follows the opposite path from blood to air.

Pneumocyte Absorption of Fluid
Because fluid along the surface of pneumocytes in alveoli presents a barrier to diffusion of gases, pneumocytes actively absorb fluid via vectorial transport to maintain a thin layer of fluid and optimize the diffusion of gases. Both type I and type II pneumocytes participate in absorption of fluid. Both cells transport sodium and chloride from airway fluid into the interstitium to generate an osmotic gradient to drive water absorption. Sodium (ENaC) and chloride (CFTR) channels in the apical surface mediate diffusion into pneumocytes and the sodium-potassium pump drives sodium into the interstitium. Water can flow paracellularly or via aquaporin channels in type I pneumocytes.

Alveolar Macrophages
Alveolar macrophages reside within the airspaces of alveoli and serve to remove particulate matter such as dust and pollen. Alveolar macrophages also called dust cells. Alveolar macrophages derive from monocytes and also exist in the connective tissue of the lung. An increase in macrophages in the airways is often an indicator of a pathologic condition.

Pulmonary Circulation
The lungs are supplied by two types of circulatory systems: pulmonary and bronchial. The bronchial circulation brings oxygenated blood to the large branches of the airway and its blood vessels resemble blood vessels in other systemic circulatory systems.

The pulmonary system brings deoxygenated blood from the right ventricle to the lung to mediate gas exchange in the alveoli. The pulmonary circulatory system has features that differ from other systemic circulatory systems. First, the arteries of the pulmonary system carry deoxygenated blood and the veins carry oxygenated blood. Second, the pulmonary system has considerably lower resistance compared to systemic resistance (about 1/10th).
The lower resistance in the pulmonary circulation is generated by a structural change in the walls of the arteries and arterioles. First, the arteries of the pulmonary circulation have relatively more elastic fibers and less smooth muscle compared to similar size arteries in the systemic circulation. Second, the arterioles in the pulmonary system contain only a partial layer of smooth muscle cells or completely lack smooth muscle. Recall that in most systemic circulatory systems, the arterioles generate the most resistance.

Lung Section
Now that you are familiar with the histological structure of the lung, this image show a section of lung that contains both bronchi, bronchioles, alveolar ducts and sacs. Note that bronchi and bronchioles have a similar structure but bronchioles lack cartilage plates. Also appreciate the close juxtaposition of the airways with the pulmonary blood vessels. Pulmonary arteries run alongside bronchi and conducting bronchioles. When a bronchus or conducting bronchiole branches, the pulmonary artery that accompanied the airway also branches sending a smaller artery to run alongside each of the new airways.
Observe that the walls of bronchioles are connected to alveoli. The tension in the walls of the alveoli helps prevent bronchioles from collapsing during expiration. Cartilage plates that surround bronchi keep bronchi open during expiration.

Structure of Alveoli and Rate of Ventilation
In addition to being the site of gas exchange, the structure and composition of alveoli are critical for ventilation into and out of the lung. Recall from the physiology lectures that movement of air into and out of the lung is largely driven by pressure differences inside the lung and the atmosphere. Because alveoli occupy the largest volume of the lung, changes in their dimensions create the pressure differences between the lung and atmosphere. Increasing the volume in alveoli, decreases pressure in the lung to draw air into the lung. Decreasing the volume in alveoli, increases pressure in the lung to push air out.
Two parameters decrease the volume of alveoli. The most significant is the surface tension at the air-water interface. This tension is reduced somewhat by surfactant. The second parameter is the connective tissue in the walls of alveoli. The connective tissue contains a mix of elastic fibers and collagen fibers. During normal inhalation and exhalation (tidal volumes), elastic fibers are the most important component in determining alveolar volume. Recall that elastic fibers stretch under tensile (pulling) forces and then recoil when those forces are removed. Thus, recoil of elastic fibers decreases the volume of alveoli during exhalation. Collagen fibers are curled in the walls of alveoli and only resist expansion of alveoli during deep inhalation when the walls of alveoli have lengthened sufficiently to uncurl the fibers. Recall that collagen fibers are much stiffer than elastic fibers and more strongly restrict alveoli from expanding.

To increase its volume during inhalation, the lung must overcome the recoil forces of the surface tension and tension generated by elastic fibers and collagen fibers in the walls of alveoli. These three parameters largely determine the compliance of the lung. Compliance is a measure of how much force is required to increase the volume of the lung. The higher the compliance, the less force required to increase the volume of the lungs. The force to increase the volume of the lungs comes from expansion of the rib cage and diaphragm which generates negative pressure in the fluid separating the pleural surface of the lung from the pleural surface of the chest cavity. Negative pressure in the intrapleural fluid generates the force to expand the volume of the lung. Note in the image above how alveoli are attached the pleural wall of the lung. Tension on the wall of the lung (generated by negative pressure in the intrapleural fluid) pulls on the walls of the alveoli to expand the alveolar space and increase the volume in the lung. The elastic recoil forces in alveoli are usually sufficient to decrease alveolar space during expiration.
Dealing with Inhaled Particles
At rest, the average person inhales 400 to 500 ml of air with each breath. This volume increases when the metabolic demand for oxygen increases. Besides gases, air contains different concentrations of small particles (10 µm and smaller) that can penetrate deep into the lung. Of most concern are particles smaller than 2.5 µm (PM2.5) because these have been found to reach alveoli and cross into interstitial tissue and blood.

The concentration of PM2.5 particles varies by geography. In the United States, air that has concentrations of PM2.5 below 35 µg/m3 is considered safe. Many locations in the world have much higher concentrations of PM2.5. For example, measurements taken from the U.S. embassy in Beijing detected PM2.5 concentrations greater than 100 µg/m3 for more than half the winter days between 2010 and 2014 and peak levels of 744 µg/m3.
The concentration of PM2.5 particles in the United States has slowly declined over that past several years, especially in the eastern states and during the winter month in western states. Unfortunately, the concentration of PM2.5 particles during the summer months in western states has not declined. One explanation for this disparity is the increase in the number of large forest fires in western states over the past several years. The increase in the number of forest fires is associated with climate change that has increased the daily average temperature in western states during the spring and summer.
PM2.5 particles have been shown to cause several pathologies. Experiments in animal models have found that PM2.5 particles generate free radicals in lung tissue which lead to cell and DNA damage. Cellular damage triggers inflammation which compromises that structure of alveoli and narrows the diameter of conducting bronchioles. In addition, inhaled particles appear to exasperate several pre-existing conditions, such as asthma, by activating inflammatory pathways and increasing airway resistance.
The lung has two mechanisms to eliminate inhaled particles. The first is to trap particles in mucus and remove mucus through the action of cilia on the epithelium. In alveoli dust cells (macrophages) patrol the air space and can eliminate inhaled particles through phagocytosis. While macrophages can clear pathways and interstitial tissue of inhaled particles, excessive activation of macrophages triggers inflammation leading to tissue damage and constriction of airways.
