Cardiac Radiology
Learning Objectives
- Overview the currently available imaging modalities to evaluate the cardiac structures
- Review their strengths and weaknesses
- Review common indications for each modality
Overview
There are several imaging modalities that can evaluate the cardiac structures including chest radiography, echocardiography, computed tomography (CT), magnetic resonance imaging (MRI), myocardial perfusion testing with nuclear medicine (MPI), and direct cardiac catheterization.
These modalities are complimentary and chosen based on the patient’s presenting symptoms and the clinical question at hand. Other considerations include radiation exposure, test and personnel availability, cost, length of examination, and the ability of the patient to tolerate the exam.
Strengths and weaknesses
Each modality has its inherit strengths and weaknesses based on the how the images are acquired and the information it provides.
Chest radiography (CXR) is an affordable examination that is readily available in most settings. Images are acquired quickly. It exposes the patient to a small amount of radiation and no intravenous contrast. It does not require extensive technologist training and it does not demand significant patient cooperation.
On the other hand, the images provided by radiography technique have low tissue resolution. A 3D volume is depicted as a 2D picture leading to superimposition of structures. The exam is not as sensitive or specific as cross sectional imaging.
Echocardiography is also an affordable and often readily available imaging test. Image acquisition takes longer and is very operator dependent. It does not expose the patient to radiation exposure and can be performed at the bedside in emergencies.
Images can accurately assess chamber size and function as well as global and regional wall motion. This test is also useful in the evaluation of the pericardium, cardiac valves, and intra-cardiac shunts. Evaluation of the right ventricle is usually suboptimal. Intravenous contrast agents are also available for enhanced border definition and shunt detection.
Computed Tomography (CT) is a more expensive test than CXR and echocardiogram. CT images are high in spatial and temporal resolution and thus provide excellent anatomic details. Advances in CT technology compensate for cardiac motion and image acquisition is relatively fast. Technologist training is required, particularly for cardiac indications. Patients need to lie supine, hold their breath for several heartbeats, have a heart rate <65 bpm, and be able to receive intravenous iodinated contrast if necessary. This test exposes patients to more radiation than CXR (10-50x increase). CT for cardiac indications is often available across the spectrum of practice locations.
Myocardial Perfusion Imaging (MPI) is a type of nuclear medicine imaging used to assess myocardial perfusion. It exposes the patient to radiation, may have limited availability, and it reliant on radiotracer supply. The image acquisition is relatively lengthy, but requires less patient cooperation compared to CT. Although the acquired images have low spatial resolution, this modality provides physiologic, rather than anatomic, information.
Magnetic Resonance Imaging (MRI) is a lengthy exam, requiring significant effort from the patient. It is not readily available and dedicated technologists are needed. The patient usually receives intravenous administration of gadolinium-based contrast medium. The acquired images are excellent for tissue characterization, but lower in spatial resolution when compared to CT. Cardiac MRI provides functional and physiological data. The patient received no radiation exposure, making this a good option for children and young adults.
Cardiac catheterization is a minimally invasive imaging technique that allows for diagnosis and treatment of coronary artery disease. It is relatively expensive and available in most hospital settings. Moderate sedation and intra-arterial iodinated contrast is administered.
Common indications for each modality
When assessing a patient with suspected cardiac pathology, the clinical team must choose the most appropriate imaging test – the test that will provide the necessary information at lowest cost while exposing the patient to minimal risk. The exposure to radiation should be more carefully weighed in young patients. Intravenous contrast media are frequently necessary, but are associated with their own inherent risks and limitations, which must be carefully considered in each patient.
Chest radiography is not a very sensitive or specific test, but it is a great screening modality, particularly in the acute setting when the “big picture” needs to be assessed. CXR can assess broad groups of abnormalities, such as cardiomegaly, CHF, pericardial and pleural effusion, and pneumonia. It is usually the first test ordered in patients presenting with cardiac symptoms, such as chest pain and shortness of breath. It can assess the cardiomediastinal silhouette and the lungs.

Echocardiography is commonly used as the first line test to assess cardiac function and chamber size, pericardial effusion, and valvular abnormalities. It is also a great modality to evaluate for intra-cardiac shunts and can suggest the presence of extra-cardiac shunting as well.
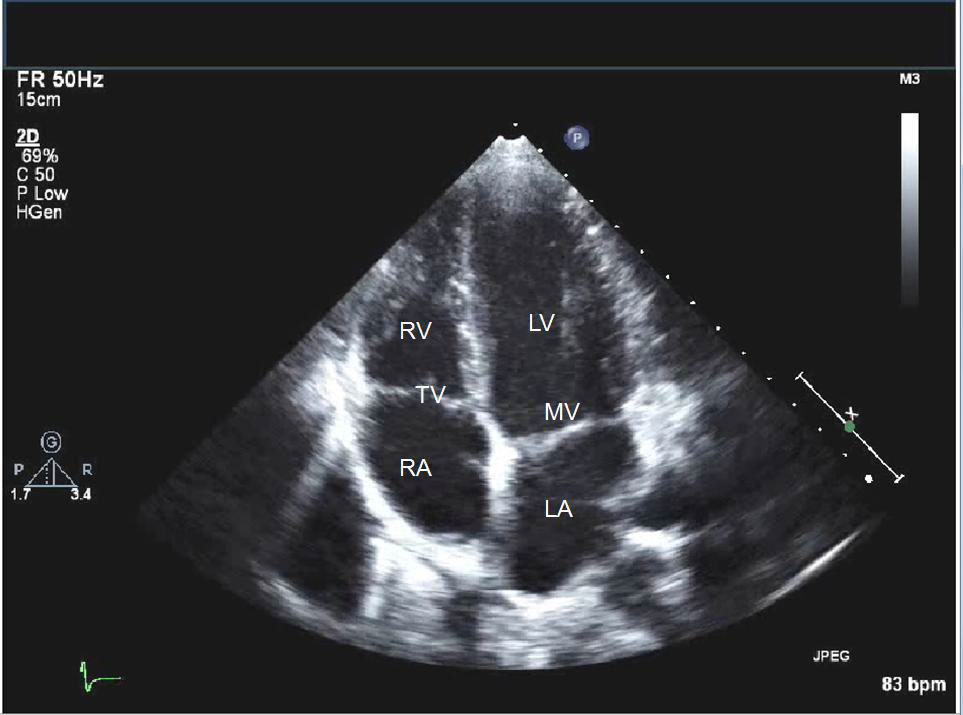
- RV - right ventricle
- TV - tricuspid valve
- RA - right atrium
- LV - left ventricle
- MV - mitral valve
- LA - left atrium
Computed Tomography can non-invasively diagnose coronary artery disease (CAD). In asymptomatic patients at low to intermediate risk for CAD, CT calcium scoring can be used to demonstrate the presence of calcified plaque. Although this non-contrast CT does not demonstrate non-calcified plaque, patients with no coronary calcium are at very low risk for a significant lesion. CT coronary angiography (CCTA), for which heart rate control and intravenous contrast is required, has excellent spatial and temporal resolution, allowing detailed visualization of the coronary vasculature. The high negative predictive value of CCTA makes it a good test to rule out CAD at the source of a patient’s symptoms. Advances in computational techniques can overcome difficulties in interpretation from excessive calcium, allowing CCTA to be used in patients at increased risk for CAD, not just those with a low pre-test probability. CCTA allows for the visualization of the myocardium and valves, and can assess function although a greater radiation dose would be necessary.


A curved planar reformatted image from a CCTA (left) demonstrates a concerning lesion in the mid LAD (arrow). On CT-FFR, a computational fluid dynamic method that uses CCTA data to determine the hemodynamic significance of stenotic lesions, the focus in question is determined to be flow-limiting with a CT-FFR value of <0.50 (normal >0.80).

Myocardial Perfusion Imaging evaluates for the functional significance of atherosclerotic lesions. However, it cannot demonstrate the presence of CAD that is not hemodynamically significant. Therefore, it is reserved for the assessment of myocardial perfusion in moderate to high-risk patients.

Magnetic Resonance Imaging is the gold standard test for the evaluation for cardiac size and function, especially of the right ventricle. MRI has the ability to characterize myocardial tissue. As such, MRI is used to evaluation myocardial viability in the setting of CAD, determining the utility of revascularization with PCI or CABG. Additionally, MRI can be used to evaluate a host of nonischemic etiologies, such as hypertrophic cardiomyopathy, sarcoidosis, amyloidosis, cardiac masses, sources of arrhythmia, and myocarditis. It is commonly used in patients with congenital heart diseases as it does not expose patients to ionizing radiation, can depict the entire chest anatomy, and can quantify shunting and valvular abnormalities. These attributes make this modality ideal for patient follow-up, particularly after surgical repair.


Cardiac catheterization is reserved for patients with acute myocardial infarction or severe coronary artery stenosis whom will likely require therapeutic intervention.
